What Can You Do About Fallen Arches?
Overview

There are many different causes of and treatments for flat foot. The most important part of treatment is determining the exact flat foot type on an individual basis, and doing so early on. The main objective is to become educated on the potential problems, so that you can stop them before they start. Conservative treatment is often successful if initiated early. The old adage "a stitch in time saves nine" definitely applies to the human body, hopefully more figuratively than literally. Do not ignore what your common sense and your body are telling you. Yes, you can live without an arch, but never neglect a symptomatic foot. If you neglect your feet, they will make you pay with every literal step you take.
Causes
The arches of most individuals are fully developed by the age of 12 to 13. While some people are born with flat arches, for others, the arches fall over time. The tibial tendon, which runs along the inside of the ankle from above the ankle to the arch, can weaken with age and with heavy activity. The posterior tendon, main support structure for the arch, can become inflamed (tendonitis) or even tear if overloaded. For women, wearing high heels can affect the Achilles tendon and alter the structure and function of the ankle. The posterior tibial tendon may compensate for this stress and break down, causing the arches to fall. Obesity is another contributing factor, as well as a serious injury to the ankle or foot, arthritis and bad circulation such as occurs with diabetes.
Symptoms
Symptoms that should be checked by a pediatrician include foot pain, sores or pressure areas on the inner side of the foot, a stiff foot, limited side-to-side foot motion, or limited up-and-down ankle motion. For further treatment you should see a pediatric orthopedic surgeon or podiatrist experienced in childhood foot conditions.
Diagnosis
Determining whether you have fallen arches may be as easy as looking at the shape of the middle bottom of your foot. Is there any kind of arch there? If you cannot find any kind of arch, you may have a flat foot. There are, however, other ways to decide in case you're still not sure. Another way to figure out if you have flat feet is to look at a few pairs of your shoes. Where do you see the most wear on the heels? If you notice significant wear in the heel and the ball of the foot extending to the big toe, this means you are overpronating. Overpronators roll their feet too far inward and commonly have fallen arches. To figure out if you have flat feet, you can also do an easy test. Get the bottoms of your feet wet and then step on to a piece of paper carefully. Step off the paper and take a look at the print your foot made. If your print looks like the entire bottom of a foot, your feet are flat. People with an arch will be missing part of the foot on their print since the arch is elevated off of the paper. Regular visits to your podiatrist are highly recommended.
What does it mean when you have flat feet?
Non Surgical Treatment
During walking and running, there is a small natural inward drop (slight pronation) that is part of the spring and propulsion. Allowing exaggerated sagging is like rounding your shoulders too much. Legs and feet have posture that you can control yourself. Use your own muscles and get free built-in exercise and arch support all day, and stop painful poor positioning. Some people with existing abnormality or growths in the ball of the foot will roll inward (or outward) to get the pressure off the deformed area because standing straight hurts. See your doctor first. Remember, don't force. If it hurts, it's wrong. All you are doing is learning how to stand neutral, not tilted so much that you compress the joints. The concept is to hold your feet in the same healthful position that shoe supports would. It is like an ice skater holds their skates straight at the ankle, not angled.
Surgical Treatment

Generally one of the following procedures is used to surgically repair a flat foot or fallen arch. Arthrodesis. One or more of your bones in the foot or ankle are fused together. Osteotomy. Correcting alignment by cutting and reshaping a bone. Excision. Removing a bone or a bone spur. Synovectomy. Cleaning the sheath that covers the tendon. Tendon transfer. Using a piece of one tendon to lengthen or replace another. Arthroereisis. placing a small device in the subtalar joint to limit motion. For most people, treatment is successful, regardless of the cause, although the cause does does play a major role in determining your prognosis. Some causes do not need treatment, while others require a surgical fix.
Prevention
Flatfeet in children are often an inherited family trait, but it may be possible to prevent the condition in some cases. Recent research has shown that there are several social or cultural factors that can cause flatfeet. These factors include the following, obesity, overweight, unnecessary orthopedic treatments, wearing rigid shoes at a young age, In 1992, a study in India of 2300 children aged 4-13 demonstrated a significant difference in the rate of flatfeet among those who wore shoes regularly and those who did not. In this study, wearing inflexible, closed-toe shoes in early childhood was shown to have a negative effect on the normal development of arches. Children who were allowed to go barefoot or who wore light sandals and slippers had a much lower rate of flatfeet. In 1999, a study in Spain of 1181 children aged 4-13 revealed that the use of orthopedic shoes for treatment of flatfeet in children not only failed to correct the problem, but actually worsened the condition by preventing the normal flexing and arch development of bare or lightly protected feet. Finally, in 2006, a study of 835 children aged 3-6 showed significant differences in the rate of flatfeet based on weight, with normal-weight children having lower rates of flatfeet than children who were overweight or obese. Among adults, flatfeet due to injury, disease, or normal aging are not preventable. However, when flatfeet are related to lifestyle factors, such as physical activities, shoe selection, and weight gain, careful attention to these factors may prevent the development of flatfeet.

There are many different causes of and treatments for flat foot. The most important part of treatment is determining the exact flat foot type on an individual basis, and doing so early on. The main objective is to become educated on the potential problems, so that you can stop them before they start. Conservative treatment is often successful if initiated early. The old adage "a stitch in time saves nine" definitely applies to the human body, hopefully more figuratively than literally. Do not ignore what your common sense and your body are telling you. Yes, you can live without an arch, but never neglect a symptomatic foot. If you neglect your feet, they will make you pay with every literal step you take.
Causes
The arches of most individuals are fully developed by the age of 12 to 13. While some people are born with flat arches, for others, the arches fall over time. The tibial tendon, which runs along the inside of the ankle from above the ankle to the arch, can weaken with age and with heavy activity. The posterior tendon, main support structure for the arch, can become inflamed (tendonitis) or even tear if overloaded. For women, wearing high heels can affect the Achilles tendon and alter the structure and function of the ankle. The posterior tibial tendon may compensate for this stress and break down, causing the arches to fall. Obesity is another contributing factor, as well as a serious injury to the ankle or foot, arthritis and bad circulation such as occurs with diabetes.
Symptoms
Symptoms that should be checked by a pediatrician include foot pain, sores or pressure areas on the inner side of the foot, a stiff foot, limited side-to-side foot motion, or limited up-and-down ankle motion. For further treatment you should see a pediatric orthopedic surgeon or podiatrist experienced in childhood foot conditions.
Diagnosis
Determining whether you have fallen arches may be as easy as looking at the shape of the middle bottom of your foot. Is there any kind of arch there? If you cannot find any kind of arch, you may have a flat foot. There are, however, other ways to decide in case you're still not sure. Another way to figure out if you have flat feet is to look at a few pairs of your shoes. Where do you see the most wear on the heels? If you notice significant wear in the heel and the ball of the foot extending to the big toe, this means you are overpronating. Overpronators roll their feet too far inward and commonly have fallen arches. To figure out if you have flat feet, you can also do an easy test. Get the bottoms of your feet wet and then step on to a piece of paper carefully. Step off the paper and take a look at the print your foot made. If your print looks like the entire bottom of a foot, your feet are flat. People with an arch will be missing part of the foot on their print since the arch is elevated off of the paper. Regular visits to your podiatrist are highly recommended.
What does it mean when you have flat feet?
Non Surgical Treatment
During walking and running, there is a small natural inward drop (slight pronation) that is part of the spring and propulsion. Allowing exaggerated sagging is like rounding your shoulders too much. Legs and feet have posture that you can control yourself. Use your own muscles and get free built-in exercise and arch support all day, and stop painful poor positioning. Some people with existing abnormality or growths in the ball of the foot will roll inward (or outward) to get the pressure off the deformed area because standing straight hurts. See your doctor first. Remember, don't force. If it hurts, it's wrong. All you are doing is learning how to stand neutral, not tilted so much that you compress the joints. The concept is to hold your feet in the same healthful position that shoe supports would. It is like an ice skater holds their skates straight at the ankle, not angled.
Surgical Treatment

Generally one of the following procedures is used to surgically repair a flat foot or fallen arch. Arthrodesis. One or more of your bones in the foot or ankle are fused together. Osteotomy. Correcting alignment by cutting and reshaping a bone. Excision. Removing a bone or a bone spur. Synovectomy. Cleaning the sheath that covers the tendon. Tendon transfer. Using a piece of one tendon to lengthen or replace another. Arthroereisis. placing a small device in the subtalar joint to limit motion. For most people, treatment is successful, regardless of the cause, although the cause does does play a major role in determining your prognosis. Some causes do not need treatment, while others require a surgical fix.
Prevention
Flatfeet in children are often an inherited family trait, but it may be possible to prevent the condition in some cases. Recent research has shown that there are several social or cultural factors that can cause flatfeet. These factors include the following, obesity, overweight, unnecessary orthopedic treatments, wearing rigid shoes at a young age, In 1992, a study in India of 2300 children aged 4-13 demonstrated a significant difference in the rate of flatfeet among those who wore shoes regularly and those who did not. In this study, wearing inflexible, closed-toe shoes in early childhood was shown to have a negative effect on the normal development of arches. Children who were allowed to go barefoot or who wore light sandals and slippers had a much lower rate of flatfeet. In 1999, a study in Spain of 1181 children aged 4-13 revealed that the use of orthopedic shoes for treatment of flatfeet in children not only failed to correct the problem, but actually worsened the condition by preventing the normal flexing and arch development of bare or lightly protected feet. Finally, in 2006, a study of 835 children aged 3-6 showed significant differences in the rate of flatfeet based on weight, with normal-weight children having lower rates of flatfeet than children who were overweight or obese. Among adults, flatfeet due to injury, disease, or normal aging are not preventable. However, when flatfeet are related to lifestyle factors, such as physical activities, shoe selection, and weight gain, careful attention to these factors may prevent the development of flatfeet.
What Causes Heel Serious Pain
Overview

Heel pain is a common foot condition. It's usually felt as an intense pain when using the affected heel. Heel pain usually builds up gradually and gets worse over time. The pain is often severe and occurs when you place weight on the heel. In most cases, only one heel is affected, although estimates suggest that around a third of people have pain in both heels. The pain is usually worse first thing in the morning, or when you first take a step after a period of inactivity. Walking usually improves the pain, but it often gets worse again after walking or standing for a long time. Some people may limp or develop an abnormal walking style as they try to avoid placing weight on the affected heel.
Causes
The two major causes of heel pain are plantar fasciitis and achilles tendinitis. The easiest way to figure out which one is causing your pain is by location. Generally speaking, if the pain is under your heel bone it is likely plantar fasciitis. If the pain is found at the back of the heel, in the achilles or toward the base of the achilles (the long cord that extends from your calf to your heel bone), then it is likely achilles tendinitis.
Symptoms
Sever?s Disease. This is a condition that occurs in 10 - 15 year old children, predominantly boys and is associated with running and repetitive jumping. It is also associated with flimsy footwear that kids may wear. It occurs when the Achilles tendon continually pulls on the apophysis of the calcaneum and does not allow for it to fuse with the body of the calcaneum. Calcaneal enthesopathy. This occurs when there is repetitive trauma at the attachment of the Achilles tendon, resulting in a spur from the calcaneum up into the Achilles tendon. It is usually visualized on x-ray and may be tender if there is an associated bursitis or tendonitis. "Pump Bump". Also known as Haglund?s Deformity, this is a bony enlargement that exists on the back of the heel - usually related to a congenital abnormality or with chronic bursitis, causing a thickening. There may have already been trauma or pressure from footwear. Treatment is usually protection of the bump and correct footwear. Associated with a symmetrical swelling at the base of the Achilles tendon. It is usually related to repetitive trauma or inappropriate footwear. It is often red and hot in the early stages. Treatment is usually to correct the footwear, provide padding and treat the local symptoms e.g. ice, rest, physiotherapy and cortisone injection. Fat Pad Syndrome. Direct contact with the base of the heel may result in trauma to the fat pad. Related to obesity, training on hard surfaces, uneven grounds, poor shoes especially overlarge shoes which can cause shearing forces on the heel. These conditions are renowned for taking a long time to recover - usually many months.
Diagnosis
The diagnosis of heel pain and heel spurs is made by a through history of the course of the condition and by physical exam. Weight bearing x-rays are useful in determining if a heel spur is present and to rule out rare causes of heel pain such as a stress fracture of the heel bone, the presence of bone tumors or evidence of soft tissue damage caused by certain connective tissue disorders.
Non Surgical Treatment
As heel pain is basically a stress problem in the tissues of the heel, the main treatment is to reduce stress. Your doctor will advise you about weight loss and appropriate footwear. A soft heel pad is useful to wear in your shoe to act as a shock-absorber when you walk. If you have a stiff ankle or tight Achilles tendon a physiotherapist can advise on exercises for these. Stretching the Achilles tendon and plantar fascia is very effective general treatment for many patients. If you have a high-arched or flat foot, a podiatrist may advise an insole to reduce stress. Simple pain-killers such as paracetamol or anti-inflammatory medicines can help reduce the pain. Ask advice from your doctor or pharmacist before taking anti-inflammatory medicines as they can have troublesome side-effects in some people. The simple measures above will help the majority of people with heel pain. If the pain continues, a splint to wear on your ankle at night to prevent your Achilles tendon tightening up while you are asleep is often very effective in improving the severe pain that many people get first thing in the morning and breaking the cycle of pain. Your GP or an orthopaedic foot and ankle surgeon or rheumatologist may inject some steroid into the attachment of the plantar fascia to damp down the inflammation. These measures will reduce the pain in most people who are not helped by simple treatment. If you still have pain after one or two injections, your doctor may want to investigate your problem a bit further. If no other medical problem or cause of stress in your heel is found, a number of other treatments can be tried. Further physiotherapy, wearing a plaster cast to rest the inflamed tissues, pain control treatments such as transcutaneous nerve stimulation (TENS) or acupuncture. Only if all non-surgical treatments fail would an operation be considered.
Surgical Treatment
Surgery is a last resort in the treatment of heel pain. Physicians have developed many procedures in the last 100 years to try to cure heel pain. Most procedures that are commonly used today focus on several areas, remove the bone spur (if one is present), release the plantar fascia (plantar fasciotomy), release pressure on the small nerves in the area. Usually the procedure is done through a small incision on the inside edge of the foot, although some surgeons now perform this type of surgery using an endoscope. An endoscope is a tiny TV camera that can be inserted into a joint or under the skin to allow the surgeon to see the structures involved in the surgery. By using the endoscope, a surgeon can complete the surgery with a smaller incision and presumably less damage to normal tissues. It is unclear whether an endoscopic procedure for this condition is better than the traditional small incision. Surgery usually involves identifying the area where the plantar fascia attaches to the heel and releasing the fascia partially from the bone. If a small spur is present this is removed. The small nerves that travel under the plantar fascia are identified and released from anything that seems to be causing pressure on the nerves. This surgery can usually be done on an outpatient basis. This means you can leave the hospital the same day.
heel pain cure
Prevention
Flexibility is key when it comes to staving off the pain associated with these heel conditions. The body is designed to work in harmony, so stretching shouldn?t be concentrated solely on the foot itself. The sympathetic tendons and muscles that move the foot should also be stretched and gently exercised to ensure the best results for your heel stretches. Take the time to stretch thighs, calves and ankles to encourage healthy blood flow and relaxed muscle tension that will keep pain to a minimum. If ice is recommended by a doctor, try freezing a half bottle of water and slowly rolling your bare foot back and forth over it for as long as is comfortable. The use of elastic or canvas straps to facilitate stretching of an extended leg can also be helpful when stretching without an assistant handy. Once cleared by a doctor, a daily regimen of over-the-counter anti-inflammatory medication like Naproxen Sodium will keep pain at bay and increase flexibility in those afflicted by heel pain. While this medication is not intended to act as a substitute for medical assessments, orthopedics or stretching, it can nonetheless be helpful in keeping discomfort muted enough to enjoy daily life. When taking any medication for your heel pain, be sure to follow directions regarding food and drink, and ask your pharmacist about possible interactions with existing medications or frequent activities.

Heel pain is a common foot condition. It's usually felt as an intense pain when using the affected heel. Heel pain usually builds up gradually and gets worse over time. The pain is often severe and occurs when you place weight on the heel. In most cases, only one heel is affected, although estimates suggest that around a third of people have pain in both heels. The pain is usually worse first thing in the morning, or when you first take a step after a period of inactivity. Walking usually improves the pain, but it often gets worse again after walking or standing for a long time. Some people may limp or develop an abnormal walking style as they try to avoid placing weight on the affected heel.
Causes
The two major causes of heel pain are plantar fasciitis and achilles tendinitis. The easiest way to figure out which one is causing your pain is by location. Generally speaking, if the pain is under your heel bone it is likely plantar fasciitis. If the pain is found at the back of the heel, in the achilles or toward the base of the achilles (the long cord that extends from your calf to your heel bone), then it is likely achilles tendinitis.
Symptoms
Sever?s Disease. This is a condition that occurs in 10 - 15 year old children, predominantly boys and is associated with running and repetitive jumping. It is also associated with flimsy footwear that kids may wear. It occurs when the Achilles tendon continually pulls on the apophysis of the calcaneum and does not allow for it to fuse with the body of the calcaneum. Calcaneal enthesopathy. This occurs when there is repetitive trauma at the attachment of the Achilles tendon, resulting in a spur from the calcaneum up into the Achilles tendon. It is usually visualized on x-ray and may be tender if there is an associated bursitis or tendonitis. "Pump Bump". Also known as Haglund?s Deformity, this is a bony enlargement that exists on the back of the heel - usually related to a congenital abnormality or with chronic bursitis, causing a thickening. There may have already been trauma or pressure from footwear. Treatment is usually protection of the bump and correct footwear. Associated with a symmetrical swelling at the base of the Achilles tendon. It is usually related to repetitive trauma or inappropriate footwear. It is often red and hot in the early stages. Treatment is usually to correct the footwear, provide padding and treat the local symptoms e.g. ice, rest, physiotherapy and cortisone injection. Fat Pad Syndrome. Direct contact with the base of the heel may result in trauma to the fat pad. Related to obesity, training on hard surfaces, uneven grounds, poor shoes especially overlarge shoes which can cause shearing forces on the heel. These conditions are renowned for taking a long time to recover - usually many months.
Diagnosis
The diagnosis of heel pain and heel spurs is made by a through history of the course of the condition and by physical exam. Weight bearing x-rays are useful in determining if a heel spur is present and to rule out rare causes of heel pain such as a stress fracture of the heel bone, the presence of bone tumors or evidence of soft tissue damage caused by certain connective tissue disorders.
Non Surgical Treatment
As heel pain is basically a stress problem in the tissues of the heel, the main treatment is to reduce stress. Your doctor will advise you about weight loss and appropriate footwear. A soft heel pad is useful to wear in your shoe to act as a shock-absorber when you walk. If you have a stiff ankle or tight Achilles tendon a physiotherapist can advise on exercises for these. Stretching the Achilles tendon and plantar fascia is very effective general treatment for many patients. If you have a high-arched or flat foot, a podiatrist may advise an insole to reduce stress. Simple pain-killers such as paracetamol or anti-inflammatory medicines can help reduce the pain. Ask advice from your doctor or pharmacist before taking anti-inflammatory medicines as they can have troublesome side-effects in some people. The simple measures above will help the majority of people with heel pain. If the pain continues, a splint to wear on your ankle at night to prevent your Achilles tendon tightening up while you are asleep is often very effective in improving the severe pain that many people get first thing in the morning and breaking the cycle of pain. Your GP or an orthopaedic foot and ankle surgeon or rheumatologist may inject some steroid into the attachment of the plantar fascia to damp down the inflammation. These measures will reduce the pain in most people who are not helped by simple treatment. If you still have pain after one or two injections, your doctor may want to investigate your problem a bit further. If no other medical problem or cause of stress in your heel is found, a number of other treatments can be tried. Further physiotherapy, wearing a plaster cast to rest the inflamed tissues, pain control treatments such as transcutaneous nerve stimulation (TENS) or acupuncture. Only if all non-surgical treatments fail would an operation be considered.
Surgical Treatment
Surgery is a last resort in the treatment of heel pain. Physicians have developed many procedures in the last 100 years to try to cure heel pain. Most procedures that are commonly used today focus on several areas, remove the bone spur (if one is present), release the plantar fascia (plantar fasciotomy), release pressure on the small nerves in the area. Usually the procedure is done through a small incision on the inside edge of the foot, although some surgeons now perform this type of surgery using an endoscope. An endoscope is a tiny TV camera that can be inserted into a joint or under the skin to allow the surgeon to see the structures involved in the surgery. By using the endoscope, a surgeon can complete the surgery with a smaller incision and presumably less damage to normal tissues. It is unclear whether an endoscopic procedure for this condition is better than the traditional small incision. Surgery usually involves identifying the area where the plantar fascia attaches to the heel and releasing the fascia partially from the bone. If a small spur is present this is removed. The small nerves that travel under the plantar fascia are identified and released from anything that seems to be causing pressure on the nerves. This surgery can usually be done on an outpatient basis. This means you can leave the hospital the same day.
heel pain cure
Prevention
Flexibility is key when it comes to staving off the pain associated with these heel conditions. The body is designed to work in harmony, so stretching shouldn?t be concentrated solely on the foot itself. The sympathetic tendons and muscles that move the foot should also be stretched and gently exercised to ensure the best results for your heel stretches. Take the time to stretch thighs, calves and ankles to encourage healthy blood flow and relaxed muscle tension that will keep pain to a minimum. If ice is recommended by a doctor, try freezing a half bottle of water and slowly rolling your bare foot back and forth over it for as long as is comfortable. The use of elastic or canvas straps to facilitate stretching of an extended leg can also be helpful when stretching without an assistant handy. Once cleared by a doctor, a daily regimen of over-the-counter anti-inflammatory medication like Naproxen Sodium will keep pain at bay and increase flexibility in those afflicted by heel pain. While this medication is not intended to act as a substitute for medical assessments, orthopedics or stretching, it can nonetheless be helpful in keeping discomfort muted enough to enjoy daily life. When taking any medication for your heel pain, be sure to follow directions regarding food and drink, and ask your pharmacist about possible interactions with existing medications or frequent activities.
Leg Length Discrepancy Right After Knee Replacement Surgery
Overview
Surgeries for LLD are designed to do one of three general things ? shorten the long leg, stop or slow the growth of the longer or more rapidly growing leg, or lengthen the short leg. Stopping the growth of the longer leg is the most commonly utilized of the three approaches and involves an operation known as an epiphysiodesis , in which the growth plate of either the lower femur or upper tibia is visualized in the operating room using fluoroscopy (a type of real-time radiographic imaging) and ablated , which involves drilling into the region several times, such that the tissue is no longer capable of bone growth. Because the epiphyseal growth capabilities cannot be restored following the surgery, proper timing is crucial. Usually the operation is planned for the last 2 to 3 years of growth and has excellent results, with children leaving the hospital within a few days with good mobility. However, it is only appropriate for LLD of under 5cm.
Causes
There are many causes of leg length discrepancy. Some include, A broken leg bone may lead to a leg length discrepancy if it heals in a shortened position. This is more likely if the bone was broken in many pieces. It also is more likely if skin and muscle tissue around the bone were severely injured and exposed, as in an open fracture. Broken bones in children sometimes grow faster for several years after healing, causing the injured bone to become longer. A break in a child's bone through the growth center near the end of the bone may cause slower growth, resulting in a shorter leg. Bone infections that occur in children while they are growing may cause a significant leg length discrepancy. This is especially true if the infection happens in infancy. Inflammation of joints during growth may cause unequal leg length. One example is juvenile arthritis. Bone diseases may cause leg length discrepancy, as well. Examples are, Neurofibromatosis, Multiple hereditary exostoses, Ollier disease. Other causes include inflammation (arthritis) and neurologic conditions. Sometimes the cause of leg length discrepancy is unknown, particularly in cases involving underdevelopment of the inner or outer side of the leg, or partial overgrowth of one side of the body. These conditions are usually present at birth, but the leg length difference may be too small to be detected. As the child grows, the leg length discrepancy increases and becomes more noticeable. In underdevelopment, one of the two bones between the knee and the ankle is abnormally short. There also may be related foot or knee problems. Hemihypertrophy (one side too big) or hemiatrophy (one side too small) are rare leg length discrepancy conditions. In these conditions, the arm and leg on one side of the body are either longer or shorter than the arm and leg on the other side of the body. There may also be a difference between the two sides of the face. Sometimes no cause can be found. This is known as an "idiopathic" difference.
Symptoms
As patients develop LLD, they will naturally and even unknowingly attempt to compensate for the difference between their two legs by either bending the longer leg excessively or standing on the toes of the short leg. When walking, they are forced to step down on one side and thrust upwards on the other side, which leads to a gait pattern with an abnormal up and down motion. For many patients, especially adolescents, the appearance of their gait may be more personally troublesome than any symptoms that arise or any true functional deficiency. Over time, standing on one's toes can create a contracture at the ankle, in which the calf muscle becomes abnormally contracted, a condition that can help an LLD patient with walking, but may later require surgical repair. If substantial enough, LLD left untreated can contribute to other serious orthopaedic problems, such as degenerative arthritis, scoliosis, or lower back pain. However, with proper treatment, children with leg length discrepancy generally do quite well, without lingering functional or cosmetic deficiencies.
Diagnosis
There are several orthopedic tests that are used, but they are rudimentary and have some degree of error. Even using a tape measure with specific anatomic landmarks has its errors. Most leg length differences can be seen with a well trained eye, but I always recommend what is called a scanagram, or a x-ray bone length study (see picture above). This test will give a precise measurement in millimeters of the length difference.
Non Surgical Treatment
To begin a path torwards a balanced foundation and reduce pain from leg length discrepancy, ask your doctor about these Functional Orthotics and procedures. Functional Orthotics have been shown to specifically reduce pain from leg length inequality, support all three arches of the foot to create a balanced foundation, maximize shock absorption, add extra propulsion, and supply more stability, enable posture correction and long-term preventive protection. Will improve prolonged effectiveness of chiropractic adjustments. Shoe or heel Lifts, Correct the deficiencies that causes imbalances in the body.

can gym help in increasing height?
Surgical Treatment
For discrepancies over five centimeters, more aggressive surgical procedures-specifically leg lengthening procedures-are typically required. The specifics of this operative procedure are beyond the scope of this informational page, but your child's physician will be able to discuss the details in reference to your child's specific problems when considered appropriate.
Surgeries for LLD are designed to do one of three general things ? shorten the long leg, stop or slow the growth of the longer or more rapidly growing leg, or lengthen the short leg. Stopping the growth of the longer leg is the most commonly utilized of the three approaches and involves an operation known as an epiphysiodesis , in which the growth plate of either the lower femur or upper tibia is visualized in the operating room using fluoroscopy (a type of real-time radiographic imaging) and ablated , which involves drilling into the region several times, such that the tissue is no longer capable of bone growth. Because the epiphyseal growth capabilities cannot be restored following the surgery, proper timing is crucial. Usually the operation is planned for the last 2 to 3 years of growth and has excellent results, with children leaving the hospital within a few days with good mobility. However, it is only appropriate for LLD of under 5cm.

Causes
There are many causes of leg length discrepancy. Some include, A broken leg bone may lead to a leg length discrepancy if it heals in a shortened position. This is more likely if the bone was broken in many pieces. It also is more likely if skin and muscle tissue around the bone were severely injured and exposed, as in an open fracture. Broken bones in children sometimes grow faster for several years after healing, causing the injured bone to become longer. A break in a child's bone through the growth center near the end of the bone may cause slower growth, resulting in a shorter leg. Bone infections that occur in children while they are growing may cause a significant leg length discrepancy. This is especially true if the infection happens in infancy. Inflammation of joints during growth may cause unequal leg length. One example is juvenile arthritis. Bone diseases may cause leg length discrepancy, as well. Examples are, Neurofibromatosis, Multiple hereditary exostoses, Ollier disease. Other causes include inflammation (arthritis) and neurologic conditions. Sometimes the cause of leg length discrepancy is unknown, particularly in cases involving underdevelopment of the inner or outer side of the leg, or partial overgrowth of one side of the body. These conditions are usually present at birth, but the leg length difference may be too small to be detected. As the child grows, the leg length discrepancy increases and becomes more noticeable. In underdevelopment, one of the two bones between the knee and the ankle is abnormally short. There also may be related foot or knee problems. Hemihypertrophy (one side too big) or hemiatrophy (one side too small) are rare leg length discrepancy conditions. In these conditions, the arm and leg on one side of the body are either longer or shorter than the arm and leg on the other side of the body. There may also be a difference between the two sides of the face. Sometimes no cause can be found. This is known as an "idiopathic" difference.
Symptoms
As patients develop LLD, they will naturally and even unknowingly attempt to compensate for the difference between their two legs by either bending the longer leg excessively or standing on the toes of the short leg. When walking, they are forced to step down on one side and thrust upwards on the other side, which leads to a gait pattern with an abnormal up and down motion. For many patients, especially adolescents, the appearance of their gait may be more personally troublesome than any symptoms that arise or any true functional deficiency. Over time, standing on one's toes can create a contracture at the ankle, in which the calf muscle becomes abnormally contracted, a condition that can help an LLD patient with walking, but may later require surgical repair. If substantial enough, LLD left untreated can contribute to other serious orthopaedic problems, such as degenerative arthritis, scoliosis, or lower back pain. However, with proper treatment, children with leg length discrepancy generally do quite well, without lingering functional or cosmetic deficiencies.
Diagnosis
There are several orthopedic tests that are used, but they are rudimentary and have some degree of error. Even using a tape measure with specific anatomic landmarks has its errors. Most leg length differences can be seen with a well trained eye, but I always recommend what is called a scanagram, or a x-ray bone length study (see picture above). This test will give a precise measurement in millimeters of the length difference.
Non Surgical Treatment
To begin a path torwards a balanced foundation and reduce pain from leg length discrepancy, ask your doctor about these Functional Orthotics and procedures. Functional Orthotics have been shown to specifically reduce pain from leg length inequality, support all three arches of the foot to create a balanced foundation, maximize shock absorption, add extra propulsion, and supply more stability, enable posture correction and long-term preventive protection. Will improve prolonged effectiveness of chiropractic adjustments. Shoe or heel Lifts, Correct the deficiencies that causes imbalances in the body.

can gym help in increasing height?
Surgical Treatment
For discrepancies over five centimeters, more aggressive surgical procedures-specifically leg lengthening procedures-are typically required. The specifics of this operative procedure are beyond the scope of this informational page, but your child's physician will be able to discuss the details in reference to your child's specific problems when considered appropriate.
Diagnosing Mortons Neuroma
Overview
 If you sometimes feel that you are "walking on a marble," and you have persistent pain in the ball of your foot, you may have a condition called Morton's neuroma. A neuroma is a benign tumor of a nerve. Morton's neuroma is not actually a tumor, but a thickening of the tissue that surrounds the digital nerve leading to the toes. Morton's neuroma occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton's neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton's neuroma is 8 to 10 times greater in women than in men.
If you sometimes feel that you are "walking on a marble," and you have persistent pain in the ball of your foot, you may have a condition called Morton's neuroma. A neuroma is a benign tumor of a nerve. Morton's neuroma is not actually a tumor, but a thickening of the tissue that surrounds the digital nerve leading to the toes. Morton's neuroma occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton's neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton's neuroma is 8 to 10 times greater in women than in men.
Causes
There are many reasons to develop a neuroma. Improper shoe gear is probably the most likely cause. Repetitive activity and excessive pressure on the ball of the foot are common. Heredity and genetic factors may also be involved. In many cases the structure of the foot may predispose the condition. Associated conditions that may cause neuroma include: bunion, hammer toes, ligament laxity, and/or a tight calf muscle. Some patients may have thinning of the fat pad on the ball of the foot, which may result in increased pressure of the nerves. Tight pointy shoes (and high heels) without padding may induce pain in the ball of the foot. Neuroma may occur suddenly, or develop over time.
Symptoms
Patients will feel pain that worsens with walking, particularly when walking in shoes with thin soles or high heels. Also, anything that squeezes the metatarsal heads together may aggravate symptoms, such as narrow shoes. A patient may feel the need to remove the shoe and rub the foot to soothe the pain.
Diagnosis
The clinical symptoms should quickly lead your doctor to suspect a neuroma. When examined, the doctor may feel a "click" which is known as Mulder's sign. There may be tenderness in the interspace. The metatarsal bones will also be examined both clinically (and often with an xray). Tenderness at one of the metatarsal bones can suggest an overstress reaction (pre-stress fracture or stress fracture) in the bone. An ultrasound scan can confirm the diagnosis and is a less expensive and at this time, at least as sensitive a test as an MRI. An x-ray does not show neuromas, but can be useful to "rule out" other causes of the pain.
Non Surgical Treatment
Orthotics and corticosteroid injections are widely used conservative treatments for Morton?s neuroma. In addition to traditional orthotic arch supports, a small foam or fabric pad may be positioned under the space between the two affected metatarsals, immediately behind the bone ends. This pad helps to splay the metatarsal bones and create more space for the nerve so as to relieve pressure and irritation. It may however also elicit mild uncomfortable sensations of its own, such as the feeling of having an awkward object under one's foot. Corticosteroid injections can relieve inflammation in some patients and help to end the symptoms. For some patients, however, the inflammation and pain recur after some weeks or months, and corticosteroids can only be used a limited number of times because they cause progressive degeneration of ligamentous and tendinous tissues.
Surgical Treatment
Interdigital neurectomy (removal of the diseased nerve) in right hands, should give satisfactory results almost all the time. Some of the reasons behind failure is when not enough nerve is dissected, mistakes in initial diagnosis, or bad handling of adjacent nerves, tendons and joint capsules during the operation. It is very common and acceptable to have some numbness in the area where the nerve used to be. This never causes any discomfort and often gets better in few years. It is crucial to address the biomechanical pathologies underlying the impingement of the nerve during and after the surgery.
 If you sometimes feel that you are "walking on a marble," and you have persistent pain in the ball of your foot, you may have a condition called Morton's neuroma. A neuroma is a benign tumor of a nerve. Morton's neuroma is not actually a tumor, but a thickening of the tissue that surrounds the digital nerve leading to the toes. Morton's neuroma occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton's neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton's neuroma is 8 to 10 times greater in women than in men.
If you sometimes feel that you are "walking on a marble," and you have persistent pain in the ball of your foot, you may have a condition called Morton's neuroma. A neuroma is a benign tumor of a nerve. Morton's neuroma is not actually a tumor, but a thickening of the tissue that surrounds the digital nerve leading to the toes. Morton's neuroma occurs as the nerve passes under the ligament connecting the toe bones (metatarsals) in the forefoot. Morton's neuroma most frequently develops between the third and fourth toes, usually in response to irritation, trauma or excessive pressure. The incidence of Morton's neuroma is 8 to 10 times greater in women than in men.Causes
There are many reasons to develop a neuroma. Improper shoe gear is probably the most likely cause. Repetitive activity and excessive pressure on the ball of the foot are common. Heredity and genetic factors may also be involved. In many cases the structure of the foot may predispose the condition. Associated conditions that may cause neuroma include: bunion, hammer toes, ligament laxity, and/or a tight calf muscle. Some patients may have thinning of the fat pad on the ball of the foot, which may result in increased pressure of the nerves. Tight pointy shoes (and high heels) without padding may induce pain in the ball of the foot. Neuroma may occur suddenly, or develop over time.
Symptoms
Patients will feel pain that worsens with walking, particularly when walking in shoes with thin soles or high heels. Also, anything that squeezes the metatarsal heads together may aggravate symptoms, such as narrow shoes. A patient may feel the need to remove the shoe and rub the foot to soothe the pain.
Diagnosis
The clinical symptoms should quickly lead your doctor to suspect a neuroma. When examined, the doctor may feel a "click" which is known as Mulder's sign. There may be tenderness in the interspace. The metatarsal bones will also be examined both clinically (and often with an xray). Tenderness at one of the metatarsal bones can suggest an overstress reaction (pre-stress fracture or stress fracture) in the bone. An ultrasound scan can confirm the diagnosis and is a less expensive and at this time, at least as sensitive a test as an MRI. An x-ray does not show neuromas, but can be useful to "rule out" other causes of the pain.
Non Surgical Treatment
Orthotics and corticosteroid injections are widely used conservative treatments for Morton?s neuroma. In addition to traditional orthotic arch supports, a small foam or fabric pad may be positioned under the space between the two affected metatarsals, immediately behind the bone ends. This pad helps to splay the metatarsal bones and create more space for the nerve so as to relieve pressure and irritation. It may however also elicit mild uncomfortable sensations of its own, such as the feeling of having an awkward object under one's foot. Corticosteroid injections can relieve inflammation in some patients and help to end the symptoms. For some patients, however, the inflammation and pain recur after some weeks or months, and corticosteroids can only be used a limited number of times because they cause progressive degeneration of ligamentous and tendinous tissues.

Surgical Treatment
Interdigital neurectomy (removal of the diseased nerve) in right hands, should give satisfactory results almost all the time. Some of the reasons behind failure is when not enough nerve is dissected, mistakes in initial diagnosis, or bad handling of adjacent nerves, tendons and joint capsules during the operation. It is very common and acceptable to have some numbness in the area where the nerve used to be. This never causes any discomfort and often gets better in few years. It is crucial to address the biomechanical pathologies underlying the impingement of the nerve during and after the surgery.
Shoe Lifts For Leg Length Discrepancy
There are actually two unique variations of leg length discrepancies, congenital and acquired. Congenital means you are born with it. One leg is structurally shorter compared to the other. Through developmental phases of aging, the human brain picks up on the walking pattern and identifies some difference. The human body usually adapts by dipping one shoulder to the "short" side. A difference of under a quarter inch is not really uncommon, require Shoe Lifts to compensate and usually won't have a serious effect over a lifetime.

Leg length inequality goes largely undiagnosed on a daily basis, however this issue is simply corrected, and can eradicate a number of incidents of back problems.
Treatment for leg length inequality commonly involves Shoe Lifts. These are cost-effective, normally costing less than twenty dollars, compared to a custom orthotic of $200 plus. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Lumbar pain is easily the most widespread health problem impacting people today. Around 80 million men and women are afflicted by back pain at some stage in their life. It's a problem which costs businesses millions of dollars annually as a result of time lost and production. Fresh and superior treatment solutions are always sought after in the hope of reducing the economical influence this issue causes.

People from all corners of the world suffer from foot ache due to leg length discrepancy. In these types of cases Shoe Lifts are usually of very useful. The lifts are capable of reducing any pain in the feet. Shoe Lifts are recommended by countless certified orthopaedic doctors.
To be able to support the human body in a healthy and balanced fashion, your feet have got a critical task to play. Inspite of that, it's often the most overlooked region in the human body. Many people have flat-feet meaning there is unequal force exerted on the feet. This will cause other parts of the body such as knees, ankles and backs to be impacted too. Shoe Lifts guarantee that appropriate posture and balance are restored.

Leg length inequality goes largely undiagnosed on a daily basis, however this issue is simply corrected, and can eradicate a number of incidents of back problems.
Treatment for leg length inequality commonly involves Shoe Lifts. These are cost-effective, normally costing less than twenty dollars, compared to a custom orthotic of $200 plus. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Lumbar pain is easily the most widespread health problem impacting people today. Around 80 million men and women are afflicted by back pain at some stage in their life. It's a problem which costs businesses millions of dollars annually as a result of time lost and production. Fresh and superior treatment solutions are always sought after in the hope of reducing the economical influence this issue causes.

People from all corners of the world suffer from foot ache due to leg length discrepancy. In these types of cases Shoe Lifts are usually of very useful. The lifts are capable of reducing any pain in the feet. Shoe Lifts are recommended by countless certified orthopaedic doctors.
To be able to support the human body in a healthy and balanced fashion, your feet have got a critical task to play. Inspite of that, it's often the most overlooked region in the human body. Many people have flat-feet meaning there is unequal force exerted on the feet. This will cause other parts of the body such as knees, ankles and backs to be impacted too. Shoe Lifts guarantee that appropriate posture and balance are restored.
The Causes Of Heel Spur

Overview
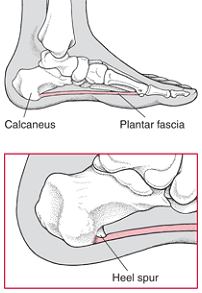
Heel Spurs are deposits of calcium in the heel area of the foot that are the typically the result of tension, abrasion and/or inflammation in the plantar fascia attachment to the heel. The heel spur itself is said not to be painful. The pain likely arises from the inflammation of the plantar fascia. The plantar fascia encapsulates muscles in the sole of the foot. It supports the arch of the foot by acting as a bowstring to connect the ball of the foot to the heel. Common causes of heel spurs include excessive load on the foot from obesity or a sudden increase in weight, a sudden increase in walking or sports activities.
Causes
Heel spurs develop in some people that have a condition called plantar fasciitis, inflammation of the plantar fascia. Heel spurs form when the plantar fascia separates from the calcaneus. An abnormal bone growth, a hook-like spur, forms from calcium deposits that grow at the site of inflammation. Heel spurs are more common in middle-aged adults and people that have had plantar fasciitis for a long time. People with flat feet or high arches are vulnerable to heel spurs. Women who wear high-heeled shoes are more susceptible, as well.
Symptoms
Major symptoms consist of pain in the region surrounding the spur, which typically increases in intensity after prolonged periods of rest. Patients may report heel pain to be more severe when waking up in the morning. Patients may not be able to bear weight on the afflicted heel comfortably. Running, walking, or lifting heavy weight may exacerbate the issue.
Diagnosis
Most patients who are suffering with heel spurs can see them with an X-ray scan. They are normally hooked and extend into the heel. Some people who have heel spur may not even have noticeable symptoms, although could still be able to see a spur in an X-ray scan.
Non Surgical Treatment
FIRST, Reduce the acute pain. This is done by a combination of several things; injection of a synthetic relative of cortisone into the heel, a prescription of anti-inflammatory pills to reduce inflammation, physical therapy and a special heel pad. About 50% of the time, these treatments will permanently relieve the pain. In the other 50%, the pain becomes recurrent, and the treatment proceeds to Stage II. SECOND, Recurrent, painful heel spur is caused by the tug and pull of the plantar fascia ligament on the heel bone with each step. When the pain is recurrent, arch supports are made to prevent sagging of the arch. The arch supports are custom-made according to the size and shape of the feet. This prevents the arch from sagging and the ligament from tugging and pulling on the heel bone. The inflammation and pain eventually go away as the first phase of treatment is continued along with the arch supports, although the spur itself remains. THIRD, Surgery to remove the spur is possible and is usually done as Day Surgery.
Surgical Treatment
Surgery, which is a more radical treatment, can be a permanent correction to remove the spur itself. If your doctor believes that surgery is indicated, he will recommend an operation - but only after establishing that less drastic methods of treatment are not successful.
Prevention
o help prevent heel and bone spurs, wear properly designed and fitted shoes or boots that provide sufficient room in the toe box so as not to compress the toes. They should also provide cushioning in appropriate areas to minimize the possibility of the irritation and inflammation that can lead to bone spurs in the feet. If needed, use inserts that provide arch support and a slight heel lift to help ensure that not too much stress is placed on the plantar fascia. This helps to reduce the possibility of inflammation and overstress. Wearing padded socks can also help by reducing trauma. Peer-reviewed, published studies have shown that wearing clinically-tested padded socks can help protect against injuries to the skin/soft tissue of the foot due to the effects of impact, pressure and shear forces. Also consider getting your gait analyzed by a foot health professional for appropriate orthotics. If you have heel pain, toe pain or top-of-the-foot pain, see your doctor or foot specialist to ensure that a spur has not developed.
What May Cause Posterior Calcaneal Spur

Overview
Heel Spurs are deposits of calcium in the heel area of the foot that are the typically the result of tension, abrasion and/or inflammation in the plantar fascia attachment to the heel. The heel spur itself is said not to be painful. The pain likely arises from the inflammation of the plantar fascia. The plantar fascia encapsulates muscles in the sole of the foot. It supports the arch of the foot by acting as a bowstring to connect the ball of the foot to the heel. Common causes of heel spurs include excessive load on the foot from obesity or a sudden increase in weight, a sudden increase in walking or sports activities.
Causes
Heel spurs can be caused by several things. Anything that can cause the body to rebuild itself can lead to a bone spur. A heel spur is a natural reaction of the body to correct a weakness by building extra bone. One of the most common causes for the development of heel spurs is the wearing of shoes that are too tight. That?s why more women suffer from heel spurs more than men. Athletes who tend to stress their feet a lot, people are overweight who have more pressure on their lower extremities and the elderly also tend to suffer more from heel spurs.

Symptoms
Bone spurs may cause sudden, severe pain when putting weight on the affected foot. Individuals may try to walk on their toes or ball of the foot to avoid painful pressure on the heel spur. This compensation during walking or running can cause additional problems in the ankle, knee, hip, or back.
Diagnosis
A thorough medical history and physical exam by a physician is always necessary for the proper diagnosis of heel spurs and other foot conditions. X rays of the heel area are helpful, as excess bone production will be visible.
Non Surgical Treatment
Heel spurs and plantar fascitis are usually controlled with conservative treatment. Early intervention includes stretching the calf muscles while avoiding re-injuring the plantar fascia. Decreasing or changing activities, losing excess weight, and improving the proper fitting of shoes are all important measures to decrease this common source of foot pain. Modification of footwear includes shoes with a raised heel and better arch support. Shoe orthotics recommended by a healthcare professional are often very helpful in conjunction with exercises to increase strength of the foot muscles and arch. The orthotic prevents excess pronation and lengthening of the plantar fascia and continued tearing of this structure. To aid in this reduction of inflammation, applying ice for 10-15 minutes after activities and use of anti-inflammatory medication can be helpful. Physical therapy can be beneficial with the use of heat modalities, such as ultrasound that creates a deep heat and reduces inflammation. If the pain caused by inflammation is constant, keeping the foot raised above the heart and/or compressed by wrapping with an ace bandage will help. Corticosteroid injections are also frequently used to reduce pain and inflammation. Taping can help speed the healing process by protecting the fascia from reinjury, especially during stretching and walking.
Surgical Treatment
Surgery to correct for heel spur syndrome is a common procedure which releases plantar fascia partially from its attachment to the calcaneous (heel bone). This part of the surgery is called a plantar fasciotomy due to the fact the fascia is cut. This is most often done through an open procedure as any heel spur or bursa can be removed at the same time. If the spur is not removed during the surgery, it will probably be just as successful, as the large spur is not the true problem. Some physicians use an endoscopic approach (EPF) where a small camera aids the physician during surgery with typically smaller incisions on each side of your foot.